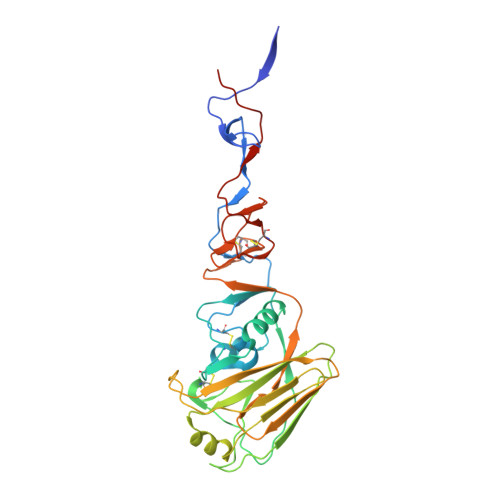
Three mutations switch H7N9 influenza to human-type receptor specificity.
de Vries, R.P., Peng, W., Grant, O.C., Thompson, A.J., Zhu, X., Bouwman, K.M., de la Pena, A.T.T., van Breemen, M.J., Ambepitiya Wickramasinghe, I.N., de Haan, C.A.M., Yu, W., McBride, R., Sanders, R.W., Woods, R.J., Verheije, M.H., Wilson, I.A., Paulson, J.C.(2017) PLoS Pathog 13: e1006390-e1006390
- PubMed: 28617868
- DOI: https://doi.org/10.1371/journal.ppat.1006390
- Primary Citation of Related Structures:
5VJK, 5VJL, 5VJM - PubMed Abstract:
The avian H7N9 influenza outbreak in 2013 resulted from an unprecedented incidence of influenza transmission to humans from infected poultry. The majority of human H7N9 isolates contained a hemagglutinin (HA) mutation (Q226L) that has previously been associated with a switch in receptor specificity from avian-type (NeuAcα2-3Gal) to human-type (NeuAcα2-6Gal), as documented for the avian progenitors of the 1957 (H2N2) and 1968 (H3N2) human influenza pandemic viruses. While this raised concern that the H7N9 virus was adapting to humans, the mutation was not sufficient to switch the receptor specificity of H7N9, and has not resulted in sustained transmission in humans. To determine if the H7 HA was capable of acquiring human-type receptor specificity, we conducted mutation analyses. Remarkably, three amino acid mutations conferred a switch in specificity for human-type receptors that resembled the specificity of the 2009 human H1 pandemic virus, and promoted binding to human trachea epithelial cells.
Organizational Affiliation:
Departments of Molecular Medicine, & Immunology and Microbiology, The Scripps Research Institute, La Jolla, CA, United States of America.